DEFINITION:
The process of the origin, development, and maturation of erythrocytes is called Erythropoiesis. similarly, Hemopoiesis or hematopoiesis is the process of origin, development and maturation of all the blood cells.
Download as erythropoiesis ppt or erythropoiesis pdf
Download as erythropoiesis ppt or erythropoiesis pdf
SITE OF ERYTHROPOIESIS
IN FETAL LIFE
In fetal life, the erythropoiesis occurs in three stages:
1. Mesoblastic Stage
During the first two months of intrauterine life, the RBCs
are produced from mesenchyme of yolk sac.
are produced from mesenchyme of yolk sac.
2. Hepatic Stage
From the third month of intrauterine life, the liver is the main
organ that produces RBCs. Spleen and lymphoid organs are also involved in erythropoiesis.
organ that produces RBCs. Spleen and lymphoid organs are also involved in erythropoiesis.
3. Myeloid Stage
During the last three months of intrauterine life, the RBCs
are produced from red bone marrow and liver.
are produced from red bone marrow and liver.
IN NEWBORN BABIES, CHILDREN AND ADULTS
In newborn babies, growing children and adults, RBCs
are produced only from the red bone marrow.
are produced only from the red bone marrow.
1. Up to the age of 20 years:
RBCs are produced from the red bone marrow of all bones (long bones and all the flat bones).
2. After the age of 20 years:
RBCs are produced from membranous bones like vertebra, sternum, ribs, scapula, iliac bones and skull bones and from the ends of long bones. After 20 years of age, the shaft of the long bones becomes yellow bone marrow because of fat deposition and loses the erythropoietic function. In adults, liver and spleen may produce the blood cells if the bone marrow is destroyed or fibrosed. Collectively bone marrow is almost equal to the liver in size and weight. It is also as active as the liver. Though bone marrow is the
site of production of all blood cells, comparatively 75% of the bone marrow is involved in the production of leukocytes and only 25% is involved in the production of erythrocytes.But still, the leukocytes are less in number than the erythrocytes, the ratio being 1:500. This is mainly because of the lifespan of these cells. The lifespan of erythrocytes is 120 days whereas the lifespan of leukocytes is very
short ranging from one to ten days. So the leukocytes need larger production than erythrocytes to maintain the required number.
site of production of all blood cells, comparatively 75% of the bone marrow is involved in the production of leukocytes and only 25% is involved in the production of erythrocytes.But still, the leukocytes are less in number than the erythrocytes, the ratio being 1:500. This is mainly because of the lifespan of these cells. The lifespan of erythrocytes is 120 days whereas the lifespan of leukocytes is very
short ranging from one to ten days. So the leukocytes need larger production than erythrocytes to maintain the required number.
PROCESS OF ERYTHROPOIESIS
 |
| erythropoiesis |
The purpose of this portion is to describe the stages of erythropoiesis in a comprehensive manner from the very beginning to the final step. The process begins from stem cells called PHSC (pluripotent hematopoietic stem cells).
Stimulation:
The process of erythropoiesis is stimulated by a kidney-derived hormone known as erythropoietin. Erythropoietin, also known as hemopoietin or hematopoietin, is able to detect hypoxia (lack of oxygen) thus burst starting the process of erythropoiesis to compensate oxygen delivery.
Stem Cells:
Stem cells are the primary cells capable of self-renewal
and differentiating into specialized cells.Hemopoietic stem cells are the primitive cells in the bone marrow, which give rise to the blood cells. Hemopoietic stem cells in the bone marrow are called
uncommitted pluripotent hemopoietic stem cells (PHSC).
PHSC is defined as a cell that can give rise to all types of blood cells. In early stages, the PHSC are not designed to form a particular type of blood cell. And it is also not possible to determine the blood cell to be developed from these cells: hence, the name uncommitted PHSC. In adults, only a few number of these cells
are present. But the best source of these cells is the umbilical cord blood. When the cells are designed to form a particular type of blood cell, the uncommitted PHSCs are called committed PHSCs. Committed PHSC is defined as a cell, which is restricted to give rise to one group of blood cells.
and differentiating into specialized cells.Hemopoietic stem cells are the primitive cells in the bone marrow, which give rise to the blood cells. Hemopoietic stem cells in the bone marrow are called
uncommitted pluripotent hemopoietic stem cells (PHSC).
PHSC is defined as a cell that can give rise to all types of blood cells. In early stages, the PHSC are not designed to form a particular type of blood cell. And it is also not possible to determine the blood cell to be developed from these cells: hence, the name uncommitted PHSC. In adults, only a few number of these cells
are present. But the best source of these cells is the umbilical cord blood. When the cells are designed to form a particular type of blood cell, the uncommitted PHSCs are called committed PHSCs. Committed PHSC is defined as a cell, which is restricted to give rise to one group of blood cells.
Committed PHSCs are of two types:
1. Lymphoid stem cells (LSC)
which give rise to lymphocytes and natural killer (NK) cells
2. Colony forming blastocytes
which give rise to myeloid cells. Myeloid cells are the blood cells other than lymphocytes. When grown in cultures, these cells form colonies hence the name colony forming blastocytes.
Different units of colony forming cells are:
i. Colony forming unit-erythrocytes (CFU-E)
Cells of this unit develop into erythrocytes
ii. Colony forming unit-granulocytes/monocytes
(CFU-GM) – These cells give rise to granulocytes
(neutrophils, basophils and eosinophils) and
monocytes
iii. Colony forming unit-megakaryocytes (CFU-M)
Platelets are developed from these cells.
Different units of colony forming cells are:
i. Colony forming unit-erythrocytes (CFU-E)
Cells of this unit develop into erythrocytes
ii. Colony forming unit-granulocytes/monocytes
(CFU-GM) – These cells give rise to granulocytes
(neutrophils, basophils and eosinophils) and
monocytes
iii. Colony forming unit-megakaryocytes (CFU-M)
Platelets are developed from these cells.
Changes that occur during erythropoiesis:
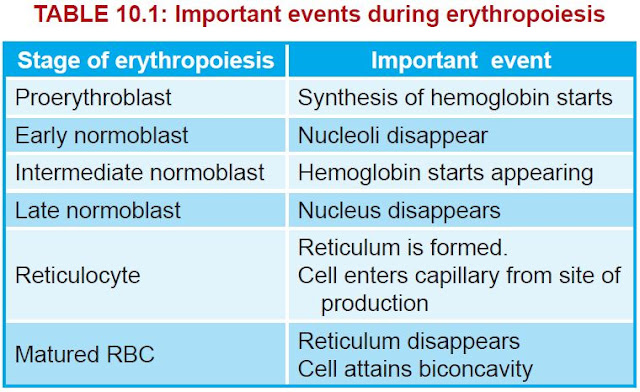
Cells of CFU-E pass through different stages and finally become the matured RBCs. During these stages, four important changes are noticed.
- Reduction in size of the cell (from the diameter of 25 to 7.2 μ)
- Disappearance of nucleoli and nucleus
- Appearance of haemoglobin
- Change in the staining properties of the cytoplasm.
Stages of erythropoiesis:
Various stages between CFU-E cells and matured RBCs
are (Fig. 10.2):
1. Proerythroblast
2. Early normoblast
3. Intermediate normoblast.
are (Fig. 10.2):
1. Proerythroblast
2. Early normoblast
3. Intermediate normoblast.
4. Late normoblast
5. Reticulocyte
6. Matured erythrocyte.
5. Reticulocyte
6. Matured erythrocyte.
Proerythroblast (Megaloblast)
Proerythroblast or megaloblast is the first cell derived from CFU-E. It is very large in size with a diameter of about 20 μ. Its nucleus is large and occupies the cell almost completely. The nucleus has two or more nucleoli and a reticular network. Proerythroblast does not contain haemoglobin. The cytoplasm is basophilic in nature. Proerythroblast multiplies several times and finally forms the cell of next stage called early normoblast. Synthesis of haemoglobin starts at this stage. However, the appearance of haemoglobin occurs only in intermediate normoblast.
Early Normoblast
The early normoblast is little smaller than proerythroblast with a diameter of about 15 μ. In the nucleus, the nucleoli disappear. Condensation of chromatin network occurs. The condensed network becomes dense. The cytoplasm is basophilic in nature. So, this cell is also called basophilic erythroblast. This cell develops into
next stage called intermediate normoblast.
Intermediate Normoblast
The cell is smaller than the early normoblast with a diameter of 10 to 12 μ. The nucleus is still present. But, the chromatin network shows further condensation. The haemoglobin starts appearing. Cytoplasm is already basophilic. Now, because of the presence of haemoglobin, it stains with both acidic as well as basic stains. So this cell is called polychromatophilic or polychromatic erythroblast. This cell develops into next stage called late normoblast.
Late Normoblast
The diameter of the cell decreases further to about 8 to 10 μ. Nucleus becomes very small with very much condensed chromatin network and it is known as the ink-spot nucleus. The quantity of haemoglobin increase. And the cytoplasm becomes almost acidophilic. So, the cell is now called orthochromatic erythroblast. In the final stage of
late normoblast just before it passes to next stage, the nucleus disintegrates and disappears. The process by which nucleus disappears is called pyknosis. The final remnant is extruded from the cell. Late normoblast develops into the next stage called reticulocyte.
late normoblast just before it passes to next stage, the nucleus disintegrates and disappears. The process by which nucleus disappears is called pyknosis. The final remnant is extruded from the cell. Late normoblast develops into the next stage called reticulocyte.
Reticulocyte
Reticulocyte is otherwise known as immature RBC. It is slightly larger than matured RBC. The cytoplasm contains the reticular network or reticulum, which is formed by remnants of disintegrated organelles. Due to the reticular network, the cell is called reticulocyte. The reticulum of reticulocyte stains with supravital stain. In newborn babies, the reticulocyte count is 2% to 6% of RBCs, i.e. 2 to 6 reticulocytes are present for every 100 RBCs. The number of reticulocytes decreases during the first week after birth. Later, the reticulocyte count remains constant at or below 1% of RBCs. The number increases whenever production and release of
RBCs increase. Reticulocyte is basophilic due to the presence of
remnants of disintegrated Golgi apparatus, mitochondria and other organelles of cytoplasm. During this stage, the cells enter the blood capillaries through the capillary membrane from the site of production by diapedesis. Important events during erythropoiesis is given in Table 10.1
RBCs increase. Reticulocyte is basophilic due to the presence of
remnants of disintegrated Golgi apparatus, mitochondria and other organelles of cytoplasm. During this stage, the cells enter the blood capillaries through the capillary membrane from the site of production by diapedesis. Important events during erythropoiesis is given in Table 10.1
Matured Erythrocyte
Reticular network disappears and the cell becomes the matured RBC and attains the biconcave shape. The cell decreases in size to 7.2 μ diameter. The matured RBC is with haemoglobin but without a nucleus. It requires 7 days for the development and maturation of RBC from proerythroblast. It requires 5 days up to the stage of reticulocyte. Reticulocyte takes 2 more days to become the matured RBC.
 |
| IMPORTANT EVENTS DURING ERYTHROPOIESIS |
see this video
incoming searches
incoming searches



